A Donor Bill of Rights

Source: WHO African Region. https://bit.ly/3lsmh8Z.
Overview of Mental Health in Africa
The African continent is a large one consisting of many nations, of which, most are low and middle-income countries (LMICs), especially in the Sub-Saharan region. Most parts of the continent are characterized by high mortality rates from malnutrition, infectious and non-infectious diseases, and a lack of basic healthcare amenities. Healthcare is one economic aspect that is poorly funded in many African countries, which is highlighted by the inability of these nations to implement the Abuja Declaration of 2001. This declaration, which was made by member countries of the African Union, involved a pledge by each country to allocate at least 15% of their national budget to the healthcare sector. Two decades after this declaration, healthcare budgetary allocation in many African countries still lags below 15%, and mental health happens to be the least considered aspect of the health sector.
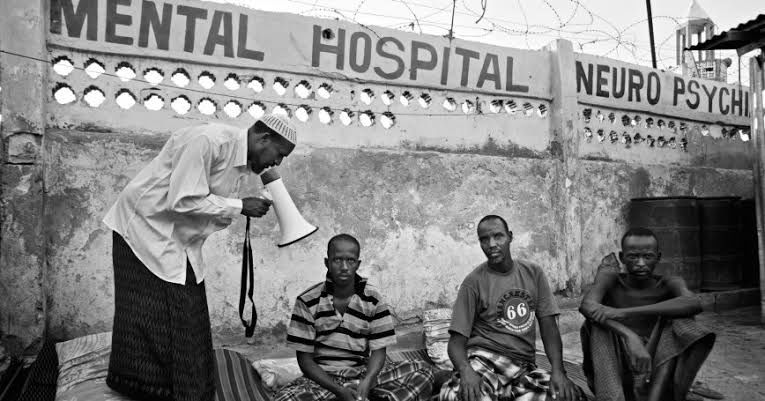
Much earlier on in 1988 and 1990, the member states of the World Health Organization (WHO) African Region had developed and adopted two public health resolutions to improve the quality of mental health services by formulating suitable mental health policies, programmes and action plans. Series of surveys since then have shown that despite some level of improvements, a lot is yet to be done about the state of mental health services in most African countries. Various misconceptions about mental health conditions are prevalent among the general public, and people’s attitudes towards mental illness are strongly influenced by traditional beliefs in the supernatural. Stigmatization against mentally challenged individuals is very common, and little is done to support such persons physically or emotionally.
Source: Rand Corporation. https://bit.ly/3cKGCSV.
Problems Associated with Mental Health in Africa
With the development of newer and more effective medications for the treatment of mental illnesses, it is expected that the management outcomes of mental cases should greatly improve, however, this is not the case in most African countries. Access to such medications is limited in these countries, mostly due to their poor purchasing power, logistical problems, and difficulties in establishing local production. A shortage of mental health workers is quite common in most African countries, as statistics show that the African region has just 1.4 mental health workers per 100,000 people, compared with the global average of about 9 mental health workers per 100,000 individuals. There is a glaring deficit of Psychiatrists in the region due to minimal professional training and low rate of specialization among doctors as a result of the associated stigma. In addition, the state of mental rehabilitation facilities is quite appalling, as the number of hospital beds for mentally ill patients is far less than the global average, which is one of the reasons why low rates of visits to mental health facilities are recorded in the region.
Though some efforts have been made to establish policies to improve the quality of mental health services, little success has been recorded with implementation, and a number of African countries outrightly lack any standalone mental health policies or programmes. This is further compounded by the deficit of substantial research into mental health problems, making it difficult to monitor the frequency of mental cases and the level of treatment inadequacies. With the absence of definitive research, there is no statistical basis for governments and policy markers to work with in order to enact and implement effective policies that suit the mental health challenges peculiar to each country. One of the consequences of the weak policy system is the nonchalant use of crude treatment methods for the management of mentally ill patients, such as beating, chaining and forceful administration of medications to patients in mental rehabilitation centers. As a result of the distressing experiences faced by these patients, it is quite common for individuals with mental health conditions to refrain from seeking medical attention, for fear of being ‘taken away’ to rehabilitation centers to receive such treatment methods.
The emergence of the COVID-19 pandemic has further worsened mental health states, not just in Africa, but on a global scale. The lockdown measures implemented by most countries served as a trigger for various mental conditions like depression, loneliness and anxiety, and also exacerbated the already existing mental disorders of indoor and outdoor patients. This has resulted in an increased demand for mental health services, which unfortunately cannot be met by many health facilities, as most healthcare efforts are currently channeled towards the COVID-19 response. As the pandemic gradually resolves, most hospitals and health facilities have been reopened, but social distancing measures are still being implemented, making it difficult to have regular physical appointments with mental healthcare givers.
Solutions to the Mental Health Security Challenges in Africa
Collective efforts must be made by all African leaders to increase the national budgetary allocation to mental healthcare in their individual countries, and also work towards setting up more rehabilitation centers that are well-equipped to adequately handle mental health cases. Public-private partnerships should be established in order to create intensified training programmes for psychiatrists and other mental health professionals, and efforts should also be made to introduce incentives into their payment scheme to encourage them in their job of caring for mentally challenged individuals. National health-related bodies and non-profit organizations (NGOs) can encourage policy making by awarding grants to African researchers for carrying out quantitative and qualitative research studies that assess the prevalence of mental disorders, the associated risk factors, the effectiveness and cost of treatment interventions, and the type of policies most suitable for responding to mental health challenges. Such research studies will enable governments and policy makers to enact and implement effective policies that will improve the quality of mental health services, and also ensure the eradication of all abusive treatment methods, while preserving the fundamental human rights of mentally ill patients in rehabilitation centers.
In a bid to improve public awareness about mental health conditions, individual African countries can make efforts to set up awareness campaigns at the local and national levels through physical means like awareness rallies and educational programmes in rural and urban communities, as well as the use of virtual means like circulation of infographics and myth busters about mental health on social media platforms and hosting television or radio programmes that educate citizens on the complexities of mental disorders and the need to preserve the dignity of mentally challenged persons. Through such physical and virtual means, people can also get access to expert medical advice on the right practices necessary to maintain their mental wellbeing, and mentally ill persons can be encouraged to seek medical help without delay.
With the advent of the COVID-19 pandemic, health systems in most developed countries have adopted the use of telemedicine in the administration of healthcare services, including those related to mental health. As the rate of telecommunication use has greatly improved in most African countries recently, similar telehealth approaches can be adopted as well. A number of mental health-focused NGOs are currently being set up across Africa such as MANI and PsyndUp in Nigeria, the MEGA project in Zambia and South Africa, Wazi in Kenya and MindIT in Ghana. These mental health tech startups have been working closely with local and national psychiatry associations to provide free virtual consultations for mentally challenged persons, thus, ensuring quicker and easier access to mental healthcare services. National and international health bodies, together with African governments, can support these initiatives with the necessary funds and equipment to encourage their efforts in ensuring that the goal of adequate mental health security is achieved.
References
1. Sankoh O, Sevalie S, Weston M. Mental health in Africa. Lancet Glob Health. 2018;6(9):e954-55. https://doi.org/10.1016/S2214-109X(18)30303-6.
2. Adepoju P. Africa turns to telemedicine to close mental health gap. Lancet Digit Health. 2020;2(11):e571-72. https://doi.org/10.1016/S2589-7500(20)30252-1.
3. Gureje O, Alem A. Mental health policy development in Africa. Bull World Health Organ. 2000;78(4):475-82. PMID: 10885166.
Designed with Mobirise html site templates